Actinic or solar keratosis is the name given to the white, pink or red 3-12mm scaly patches of skin that are seen on the scalp, forehead, face, back of the arms and hands of people with fair skin who have been exposed to sun for many years.
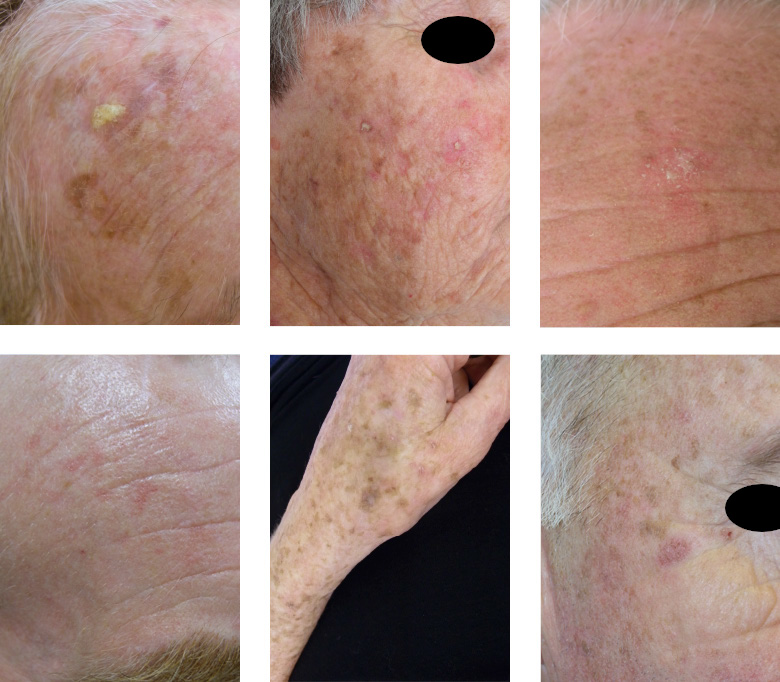
They are very common and are often felt better than they are seen. They feel like sandpaper and can prickle or itch sometimes. People often worry about them but they are harmless and are pre-malignant rather than malignant. Studies show that 0.1% of them will turn into an invasive type of skin cancer (squamous cell carcinoma) every year so it is best to have them treated.
There are several treatment options but most people choose to have them frozen with liquid nitrogen. This treatment and others are available at both clinics.
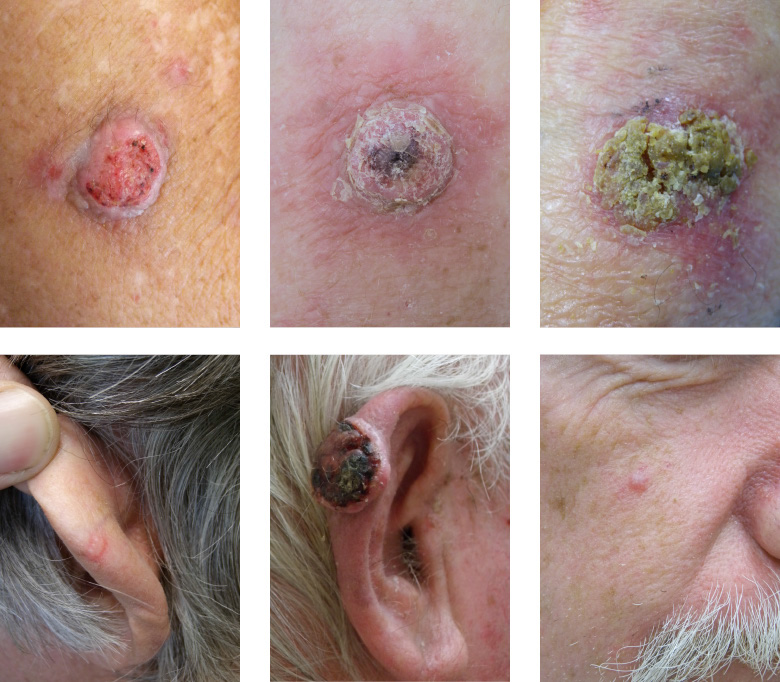
If a scaly lesion ever becomes tender, raised or bleeds, this can be a sign that it is evolving into invasive cancer and it is important to have it checked.